
By Mariana Cuervo, Elizabeth Montana, Brian Smith, and Sadie Pitzenberger
Is your local gas station attendant a drug dealer? Most people would say no, yet he readily deals all day long with customers looking for their next nicotine fix. Nicotine, the addictive substance in tobacco, keeps its users hooked.
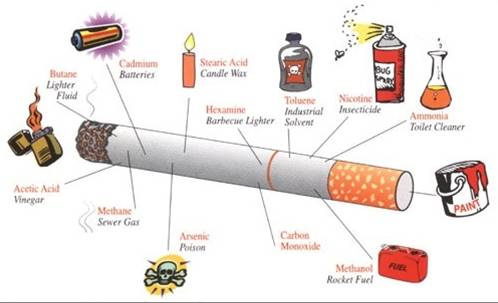
Even though most people do not consider tobacco to be a drug, this post will show that it is exactly that. Tobacco delivers similar neurobiological effects as illegal substances like cocaine, methamphetamine and marijuana, all more commonly associated with the word “drug.” With tobacco, however, advertising and the law contribute to the common perception that tobacco is not a drug.
Tobacco Products
Just like on the street corner, where you might be able to buy crack, marijuana or meth, a gas station offers different types of drugs. Tobacco itself comes in many forms: dip, snuff, cigars and, of course cigarettes.
Chewing tobacco or “dip” is a smokeless form of tobacco, which when packed into the lip allows nicotine to flow into the bloodstream via the gum line. Snuff, a finer form of tobacco, is snorted while cigarettes are smoked. Both provide an alternative way to get a nicotine high.
The ways in which these tobacco products are consumed mirror the techniques of cocaine consumption – coca leaves are chewed, cocaine is snorted, and crack is smoked. So how is tobacco different?
And just like marijuana tobacco is grown in the ground, picked and dried, and then rolled into cigars and cigarettes. Tobacco has nicotine while marijuana has tetrahydrocannabinol (THC). Both are responsible for getting the user high.


 “To this day, every time I smell firecrackers or fire arms being shot, I feel like I am right back there. All I have to do is close my eyes and I see the whole scenario over and over again. I can’t erase it.”
“To this day, every time I smell firecrackers or fire arms being shot, I feel like I am right back there. All I have to do is close my eyes and I see the whole scenario over and over again. I can’t erase it.” By Jillian Brems, Erin Brennan, Katrina Epperson, Jordan Pearce & Anna Weber
By Jillian Brems, Erin Brennan, Katrina Epperson, Jordan Pearce & Anna Weber